3D technology helps separate conjoined twins
Engineers and doctors collaborate in first successful separation of twins joined at the heart
September 1, 2017
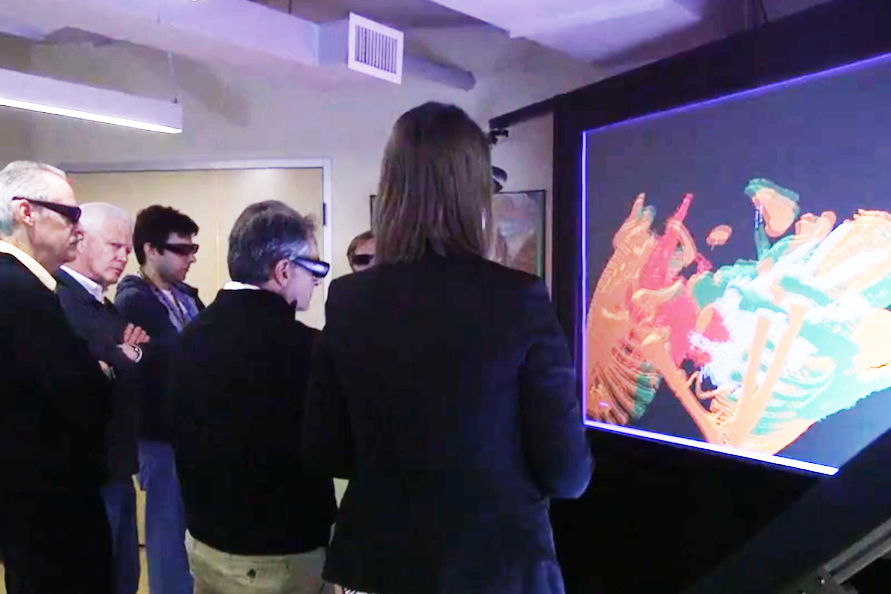
Five doctors stand in front of a large screen with a small group of engineers, staring in silence. Each wear a pair of thick, dark glasses, almost “goggle-like” in appearance.
The silence is broken: “I feel like I’m in the future right now.”
Through those glasses, they are taking a three-dimensional virtual ‘tour’ through the hearts of conjoined twin infants Paisleigh and Paislyn Martinez.
In the small group is Pediatric Surgeon Daniel Saltzman, M.D., Ph.D., a professor in the University of Minnesota Medical School's Department of Surgery. He’s tasked with separating the twin girls, whose hearts appear on the screen before him, color coded in red and blue, and enhanced more than five times in size.
From the ground up
Paisleigh and Paislyn were thoraco-omphalopagus conjoined twins—joined from the lower two-thirds of the breast bone to the belly button, although they lacked a breast bone. Their livers were fused in the middle, and their hearts appeared to be touching.
The girls’ doctors knew the only way to successfully care for the babies and their mother from prenatal care, to birth, to separation and after, was to have a team-oriented approach. Physicians from specialty areas all across the hospital met weekly with advanced practice nurse leaders. The surgical team also met several times in the operating room for ‘simulations,’ or practice runs, of the operation.
Calling on the depth of University for in-depth answers
A key component of that preparation was the expertise and collaboration of faculty and researchers at the Earl E. Bakken Medical Devices Center, a world-renowned research center within the University’s College of Science and Engineering that was recently renamed in honor of Medtronic founder and electrical engineering alumnus Earl E. Bakken. The center is home to the 3D virtual reality imaging capabilities Saltzman and the team used to visualize the Martinez twins’ hearts. The 3D virtual reality device is one of just five in the world.
“Just like a 3D movie, these virtual environments are able to show in-depth information about anatomy that is not available on a standard computer screen,” said Bethany Tourek, a mechanical engineering Ph.D. student with the Earl E. Bakken Medical Devices Center.
The 3D technology allowed doctors to virtually walk into the girls’ hearts.
“When you get into complex situations, even the most skilled radiologists and surgeons can benefit from being able to scan through the anatomy in whatever direction they want in real time,” said Art Erdman, a mechanical engineering professor and director of the University’s Earl E. Bakken Medical Devices Center. “They can enlarge it, turn it around and try to understand the complexities.”
Tourek worked with the medical team to create a computed tomography angiography (CTA) of each twin's anatomy. She reached out to the University of Minnesota Visible Heart Laboratory to ensure the anatomy anomalies were segmented correctly. A handful of separate models were created detailing the twins’ skeletal structures, lungs and heart cavities.
“The surgeons were able to explore the twins’ anatomy and make the appropriate plan before the procedure began. I like to think that we offered a service that improved the outcome of the twins,” Tourek said.
The surgeons agree. For starters, that technology coupled with 3-D models of the babies’ hearts revealed what they couldn’t see before: an actual physical connection bridging the two girls’ hearts.
“It was scary,” said Pediatric Cardiologist Matthew Ambrose, M.D., assistant professor in the Medical School's Department of Pediatrics. He vividly remembers the moment he saw the connection. “There were multiple reports of other babies with that connection who died during surgery. But I suspect it’s because it wasn’t recognized before surgery.”
Thinking on their feet
Fortunately, it was recognized, and that allowed the team to better prepare for the surgery – adapting their approach to accommodate the complexities unique to Paisleigh and Paislyn.
“What we had to do was separate the moderate to large communication,” explained pediatric cardiothoracic surgeon Tony Azakie, M.D., a professor and chief of the Division of Pediatric Cardiac Surgery. “My thinking was if we approach it as originally planned, then we would have to push the hearts away to access that bridge which would be located in the back and that may have caused them to become unstable. It may have compromised their circulation. So our strategy then changed.”
The surgical team decided to flip the orientation of the twins 180 degrees. Their original plan had Paisleigh staying in the OR while her sister was taken to a different operating room. Now, Paislyn would stay. Since Paislyn was born with a complex congenital heart defect, called tricuspid atresia with transposition of the great vessels and a ventricular septal defect, surgeons were planning to perform an additional surgery on Paislyn after separation. But with the new information about the heart bridge and a new surgical approach, the team had to bring additional cardiac resources and team members into the room to address Paislyn’s other heart problems.
“We anticipated every little problem we were going to have,” Saltzman said.
“We had everything down to where we were going to put monitors, how we were going to transport them, to how we were going to close the skin, and put the dressings on,” Saltzman added.
It takes a village
On May 25, 2017, at 6:30 a.m., all the preparation and planning was put to the test. Nine hours later, Paislyn and Paisleigh were successfully separated and on the road to recovery.
“I think there was an element of not knowing what we were going to encounter, but at the same time that was balanced with the fact that we had spent a lot of time planning and imaging so we did have a certain understanding of what we were going to find, and how we were going to find it,” Azakie said.
“The 3D modeling and some of the other imaging really helped us prepare for that,” Azakie added.
And it will continue to prepare others. Performing a conjoined twins separation surgery is rare. The innovative thinking, collaboration and cooperation it required could be applied to many future medical cases, and that wisdom will be passed on to health sciences students, Minnesota’s future health care leaders.
“When you have the right team almost anything is possible,” said Ambrose, looking back. “I’m still kind of in awe of the trust their parents placed in us, knowing this is something we’re inventing from the ground up. To know they trusted us to do this was very humbling.”
Story written by Krystal Barbour
About the Earl E. Bakken Medical Devices Center
The Earl E. Bakken Medical Devices Center is an interdisciplinary center in the College of Science and Engineering under the Institute for Engineering in Medicine. The center was renamed in July 2017 in honor of electrical engineering alumnus and Medtronic founder Earl E. Bakken in recognition of his support of the University and his field-shaping legacy.
The center combines research, education and training focused on medical devices. The center has successfully supported researchers through the process of moving devices from concept to market. It also works to train and support the next generation of innovators who will go on to change health care with further discoveries, following the model initiated by Bakken himself.
The Medical Devices Center was established in 2008 and was originally located in the Shepherd Labs building on the East Bank Campus. After outgrowing that location, the center moved to its current 8,000-square-foot home located in the University's Mayo Building in April 2013.
If you'd like to support innovations within the College of Science and Engineering, visit the CSE giving web page.
