Efie Kokkoli: Tiny technology treats big disease
Professor taps DNA nanotechnology to fight cancer
March 25, 2018
Cancer researchers have been intrigued recently by the promise of manufacturing nontoxic DNA nanoparticles a fraction the size of a human cell as vehicles to carry drugs into cancer cells.
But constructing nanoparticles of the right size and shape with an affinity for cancer cells is tricky, especially to reach a brain tumor.
Nanoparticles that are too large won’t cross the blood-brain barrier, the semipermeable membrane that separates circulating blood from extracellular fluid in the brain. Some shapes of nanoparticles are less effective than others in latching onto cancer cells.
A commonly used method of constructing nanoparticles, known as “DNA origami,” requires specialized software, hundreds of single-stranded DNS (ssDNA) sequences, precise control of temperature, and specific ions in the solution in which they’re made. Some nanoparticles tend to fall apart in the bloodstream before they can reach the cancer cells.
Water-loving DNA tubes
Efie Kokkoli, a professor of chemical engineering and materials science, is the lead researcher on a state-funded Minnesota Discovery, Research and InnoVation Economy (MnDRIVE) Transdisciplinary Research Program to use breakthrough DNA nanotechnology to engineer and evaluate materials that address a major health challenge.
The team of researchers, spanning many academic disciplines, has set out to use single-stranded DNA as DNA nanotubes to target and treat brain tumors.
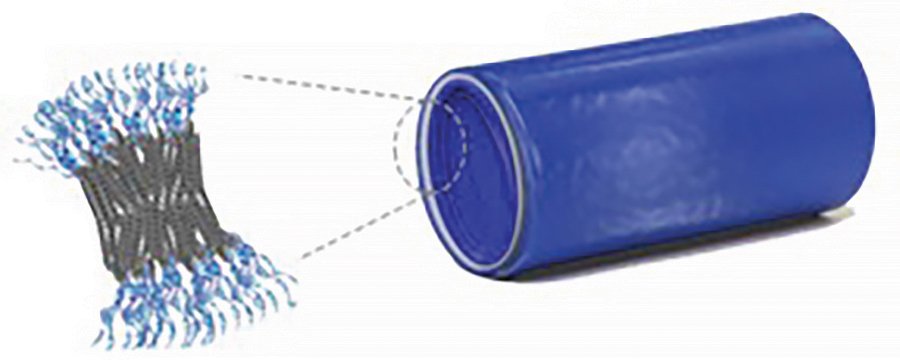
Kokkoli has recently developed a method of forming self-assembling nano-sized DNA tubes that are easy to make and stable in the bloodstream. They bind and enter cancer cells but don’t seem to enter healthy cells.
The ssDNA-amphiphiles are ssDNA sequences that love water, and conjugated to a tail that hates water. In water, these molecules self-assemble into a sphere.
Kokkoli discovered that by inserting a polycarbon “spacer” of 12 carbon atoms or more into the sequence, the amphiphiles form a tube about 30 nanometers across and about 150 nanometers long. (A nanometer is one-billionth of a meter.)
The size and tube shape make all the difference.
Fighting the right cells
Compared with other nanoparticles, the skinny tubes more easily cross the blood-brain barrier when injected into mice with brain tumors. They ranged from two to 20 times as effective as spherical nanoparticles at crossing the blood-brain barrier of mice with brain tumors.
The tubes also have much greater affinity for cancer cells than spheres. The tubes “bind and internalize,” Kokkoli said. Yet the nanotubes don’t seem to enter healthy cells.
Working on mice with brain tumors, Kokkoli said, “we see that the nanotubes are retained only on the side of the brain that has the tumor, not on the healthy side.”
So far, she doesn’t know why.
“All we can say now is that one shape works and the other shape doesn’t work at all,” Kokkoli said.
Whatever the reason, the affnity of the ssDNA nanotubes for cancer cells is a promising step in fighting the disease. By packing cancer-fighting molecules into the nanotubes, researchers may have an effective vehicle for delivering drugs into cancer cells—and only cancer cells.
The next step will be to pick candidate drugs, pack them into the tubes, and test the “therapeutic payloads” in the lab and then in animals.
“It has to be demonstrated that you can also do the therapy,” Kokkoli said. “The logical question is whether this works with other cancer types—not just brain cancer. We don’t know. We need to test them on a wider range of cancer cells.”
Story by Greg Breining
Related stories
Chad Myers: Exploring genetic connections in breast cancer
David Odde and Paolo Provenzano: Predicting cancer cell movement
If you'd like to support innovations within the College of Science and Engineering, visit the CSE giving web page.
