Fighting SARS CoV-2 at the molecular level
CSE team engineering proteins that could block coronavirus infection
May 26, 2020
Hundreds of companies and universities worldwide are racing to create a coronavirus vaccine that will equip our immune systems to fight back against the SARS CoV-2 virus, should it enter our bodies and hijack our cells.
But, what if the virus couldn’t even get into our cells?
That is the goal of College of Science and Engineering professors Ben Hackel and Jonathan Sachs, who are working with researchers in the University of Minnesota’s College of Pharmacy and Medical School to tackle COVID-19 with a molecular strategy.
Their team aims to develop and manipulate molecules that can prevent the coronavirus from attaching to human cells. If effective, this method would take the burden off the immune system to prevent infection at its core.
Lock and key
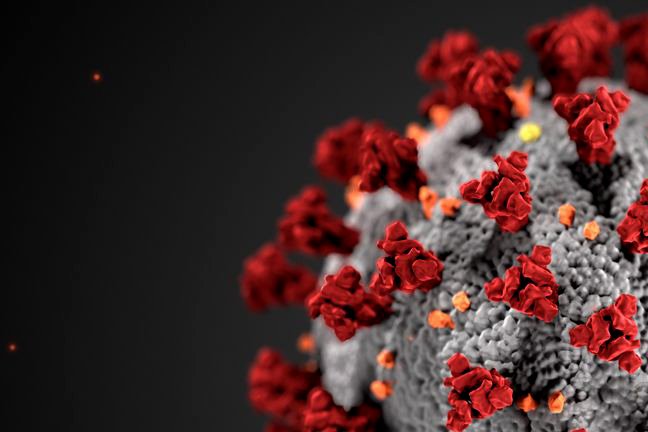
SARS CoV-2, the virus that causes COVID-19, displays spike proteins on its surface. It infects human cells by attaching the spike proteins to receptors on the surface of cells, much like a key slides into a lock.
The CSE researchers are developing two different molecules to stunt this process. One is a protein that would connect to the spike protein, blocking it from fitting into the keyhole.
“If you imagine going up to your house and taking your keys out, you’ve got to put your key in the door so it unlocks,” said Sachs, a professor in the Department of Biomedical Engineering. “The virus has to do that. The spike protein is kind of like the key."
"We’re trying to cover the key with Krazy glue so that when you’re trying to put the key in the lock, it won’t go in," he said. "The virus would just bounce off.”
The other molecule would inhibit a specific human enzyme that allows the virus to infect cells. If that enzyme is deactivated, the spike proteins wouldn’t be able to attach.
Hackel, an associate professor in the Department of Chemical Engineering and Materials Science, said the challenge is figuring out how to “turn off” the enzyme in a way that only affects viral infection.
“This family of enzymes does a lot of good things in healthy biology, so we can’t just stop all enzyme activity,” he explained. “We’d have tons of side effects. So, we’re trying to come up with a strategy to deactivate that one enzyme that’s so vital to the virus but not vital to the rest of our healthy biology.”
The protein engineering technology in Hackel’s lab allows the researchers to generate billions of molecules at a rapid pace. If they’re successful, these molecules could be developed into a treatment for people who already have COVID-19 or used as a preventative strategy for those who haven’t been infected.
It takes a village
Hackel and Sachs have been working together for the past couple of years. Funded by two grants from the National Institutes of Health, they have used similarly engineered proteins to block receptors that cause cell death in patients with non-alcoholic fatty liver disease.
When the COVID-19 pandemic hit, the pair saw another opportunity to combine their respective expertise in protein engineering and biophysics for the benefit of the nation’s public health.
“I think it grew from our ongoing collaboration to using the same fundamental technology to see if we could make a contribution in this case,” Hackel said.
“The idea of a vaccine is that you can train the immune system to [fight the virus]," he said. "We’re trying to do it from a design-build perspective.”
Hackel and Sachs are quick to note that their work wouldn’t be possible without the previous research done on relevant enzymes and how the spike protein interacts with the host cell—or without their multidisciplinary team.
The two College of Science and Engineering colleagues are working closely with medicinal chemistry professor David Ferguson in the College of Pharmacy and Alon Herschhorn, an assistant professor in the Medical School’s Division of Infectious Diseases and International Medicine.
“It takes a village,” Sachs said. “We’re trying to invent something that no one has ever invented before, and it’s something we can’t see with our eyes. In order to know that what we’re building is going to be effective, we need lots of different kinds of instruments and expertise. None of us can do that on our own.”
Sachs and Hackel said they’re also indebted to the members of their labs who do the “hard work,” and to the University of Minnesota for opening its doors to essential research during quarantine.
“It’s been essential that the University has allowed Covid research to continue,” Sachs said.
“The graduate students, postdocs, and research scientists in the labs who have risked their own personal safety to be in the lab, to carry this research out, need to be celebrated as heroes,” he said.
The right answer?
Through it all, Hackel and Sachs are staying humble. While they’ve had success in the past, there’s no guarantee this method will serve as the solution to the COVID-19 pandemic.
“We’re just trying our own aspect of things,” Hackel said. “Hopefully, we get multiple solutions as a scientific community."
"Whatever works, works, and we’re just happy to see that," he added. "This is one piece that we’re trying.”
Even if their project isn’t completed in time to help mitigate the COVID-19 crisis, the researchers believe their findings will be useful in fighting future viral outbreaks, especially coronaviruses with similar structure to SARS CoV-2.
“We’re trying to make as much progress on this as we can with the hopes of having an impact,” Hackel said. “But the long-term goal is to have a platform technology so that when future [pandemics] inevitably happen, we are prepared as a community to handle them.”
Story by Olivia Hultgren
If you'd like to support this work and other COVID-19-related activities, visit the CSE Response Fund.
